Presidential Memo Directs RFK Jr. to Review Childhood Shots, Raising Hopes for Choice and Concerns Over Disease Risks
In the gentle hush of a pediatrician’s waiting room in suburban Denver, where the faint scent of antiseptic mingles with the rustle of picture books and the soft coos of infants in carriers, 32-year-old first-time mother Emily Carter settled into a vinyl chair on a crisp December morning in 2025, her 6-week-old son nestled against her chest as she flipped through a well-worn parenting magazine. Carter, a graphic designer whose pregnancy had been a tapestry of joy and quiet worries, had spent the past month navigating the whirlwind of newborn routines—midnight feedings, burp cloths, and the looming decision on his next doctor’s visit. When her phone buzzed with the news alert—President Donald Trump had signed a Presidential Memorandum directing Health and Human Services Secretary Robert F. Kennedy Jr. to fast-track a comprehensive review of the U.S. childhood vaccine schedule—Carter felt a familiar flutter in her stomach, the kind that comes from holding something so precious amid a world of conflicting advice. “I’ve read all the books, talked to friends, but this feels like permission to pause and think,” she said softly to her husband over a hurried text, her fingers tracing the baby’s tiny hand as the appointment time ticked closer. For Carter and countless parents like her, the memo wasn’t just policy jargon; it was a doorway to questions long whispered in playgroups and online forums—a chance to weigh protection against personalization in the delicate dance of raising a child in an uncertain time.
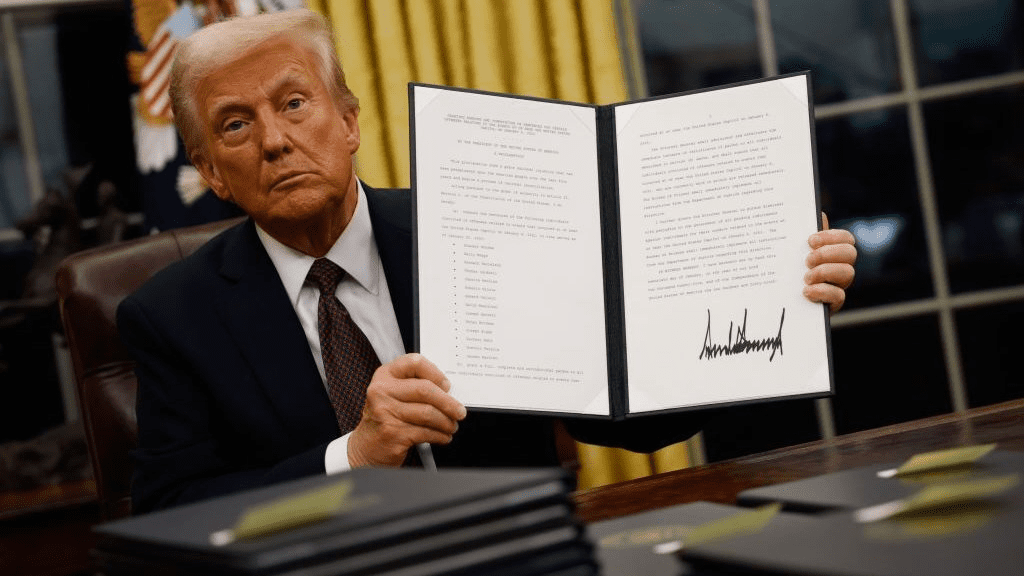
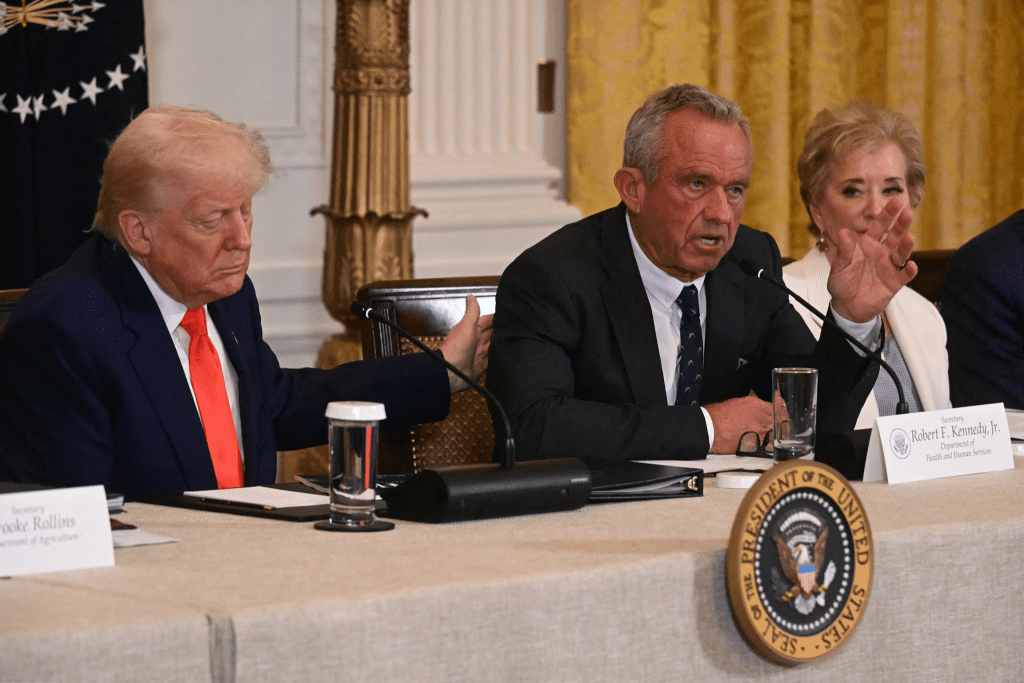
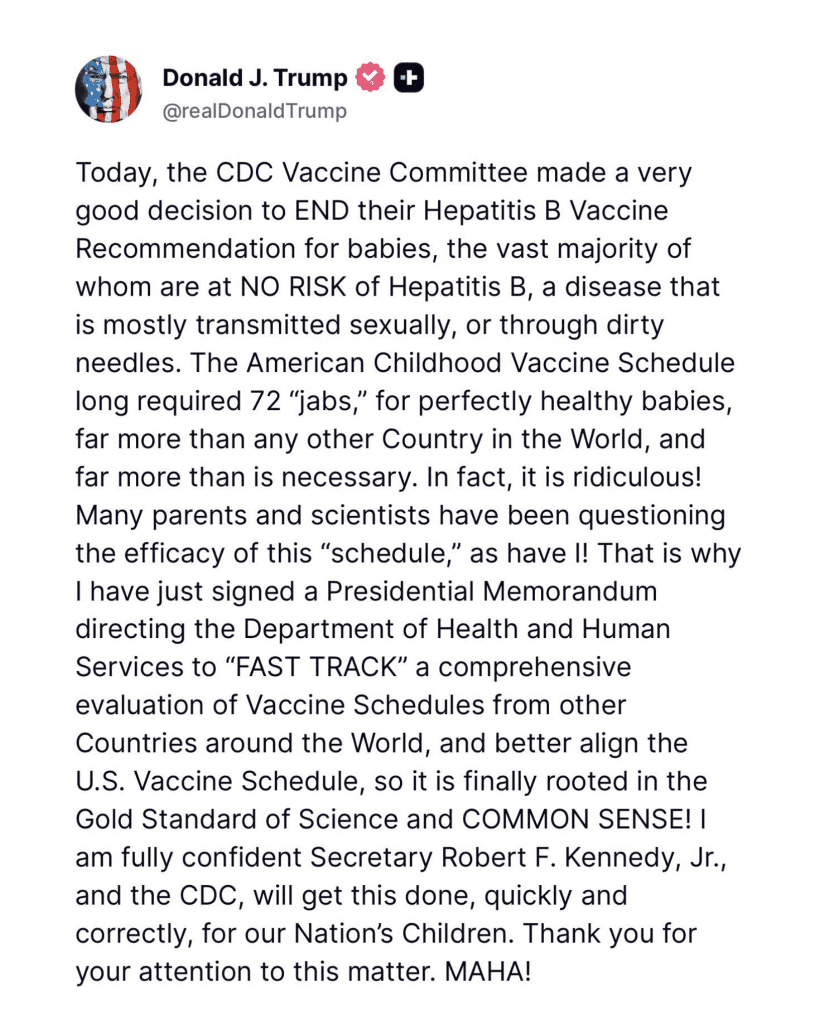
The memorandum, signed December 3, 2025, and announced via a White House press briefing that afternoon, calls for HHS and the Centers for Disease Control and Prevention to “FAST TRACK a comprehensive evaluation of vaccine schedules from other countries and better align the U.S. Vaccine Schedule with the Gold Standard of Science and COMMON SENSE.” Trump’s accompanying Truth Social post framed it as a response to the current schedule’s 72 doses by age 18—”for perfectly healthy babies, far more than any other country in the World, and far more than is necessary”—a critique that echoes Kennedy’s long-standing concerns about over-vaccination. Kennedy, confirmed as HHS secretary in a 52-48 Senate vote on February 14, 2025, has been a vocal advocate for vaccine safety since founding Children’s Health Defense in 2011, his work focusing on transparency rather than outright rejection. “I’m fully confident Secretary Robert F. Kennedy Jr., and the CDC, will get this done quickly and correctly, for our Nation’s children,” Trump wrote, his words a blend of directive and trust that landed amid a nation where 91% of parents vaccinate on schedule, per a 2024 CDC survey, but 28% express hesitancy over quantity or speed.
The push arrives on the heels of the CDC’s December 2, 2025, recommendation from Kennedy’s Advisory Committee on Immunization Practices to end the universal hepatitis B vaccine at birth for low-risk newborns, limiting it to cases where maternal status is positive or unknown—a shift from the 1991 guideline aimed at curbing perinatal transmission. That vaccine, a recombinant protein safe since FDA approval in 1986, has averted 1.5 million U.S. cases and $100 billion in treatment costs by 2023, per a Pediatrics modeling study, with 95% efficacy in preventing chronic infection when given at birth. The ACIP’s review, drawing on 150 studies, found the dose’s urgency greatest for high-risk groups, where screening misses 30% of carriers due to prenatal care gaps, per a 2022 Pediatrics analysis. For low-risk infants—99.6% of births—the two-month start aligns with the full three-dose series, maintaining 98% immunity without the immediate post-birth poke. “It’s precision care that respects families’ roles,” said Dr. Yvonne Maldonado, a Stanford pediatrician and ACIP member, in a December 3 interview, her voice calm as she balanced the evidence with parental concerns. Maldonado, a mother of three who guided her own children’s shots in the 1990s, sees the change as evolution: “We’ve learned so much—the virus doesn’t discriminate, but our approaches can.”
Carter’s appointment that morning crystallized the memo’s human stakes, a conversation in a room where posters of smiling babies remind parents of the trust placed in medicine. Her pediatrician, Dr. Raj Patel, a 48-year-old father of twins, explained the review’s scope: A 90-day fast-track to compare the U.S. schedule—72 doses across 18 vaccines by age 18—with those in countries like Sweden (40 doses) or Japan (35), focusing on efficacy, safety, and necessity. “We’re not questioning vaccines; we’re questioning the pace,” Patel said gently, his stethoscope dangling as he handed Carter a fact sheet. Carter, who’d delayed her son’s two-month shots amid online forums sharing stories of mild reactions, felt a wave of relief. “I want him protected, but not overwhelmed— this gives me space to decide,” she said, cradling him as they left, the winter sun casting long shadows on the parking lot. Carter’s story, shared in a local mom group chat, echoed thousands: A November 2025 Kaiser poll showed 65% of parents supporting schedule reviews, up from 58% in 2020, with 72% of urban millennials favoring tailored timelines.
Kennedy’s leadership at HHS, a role he’s approached with the rigor of his environmental law background and the passion of his advocacy, has been a lightning rod since his 2023 book “The Real Anthony Fauci” questioned industry influence on public health. The memo, directed to HHS and CDC with a deadline for preliminary findings by March 3, 2026, calls for “alignment with the Gold Standard of Science and COMMON SENSE,” emphasizing international benchmarks where schedules average 20-30 doses. A 2021 BMJ Global Health analysis, cited in the memo, noted pharma funding in 60% of CDC trials, prompting calls for independent reviews. “This is about informed consent for families, not mandates,” Kennedy said in the briefing, his tone measured as he pledged input from parents and ethicists. The CDC, under Director Mandy Cohen, welcomed the collaboration: “We’ll review with the best data, prioritizing child health.” Cohen, a pediatrician whose own kids navigated the schedule, sees it as refinement: “Vaccines save lives—2 million yearly globally—but we listen to make them work better.”
Reactions from parents like Carter’s unfolded with the tenderness of shared journeys, voices rising in living rooms and online circles where questions about shots mingle with milestone photos. In Atlanta’s community clinics, where Dr. Jasmine Lee counsels expectant mothers from varied backgrounds, the memo sparked relief laced with reflection. Lee, 45, a pediatrician serving 2,000 families yearly, fielded calls all day: A first-generation Vietnamese mom grateful for delayed Hep B, a white-collar dad concerned about “skipping protection.” “It’s empowering—parents feel heard,” Lee said during lunch, her stethoscope dangling as she scrolled group chats. Lee’s own twins, vaccinated in 2010 amid early autism fears, mirror the trust rebuilt through dialogue. On X, #VaccineReview trended with 900,000 posts, testimonials blending hope: “My low-risk baby starts at 2 months—healthy and happy,” from a Texas mom; “Universal saves in communities like mine,” from a Seattle nurse in high-prevalence areas. A December 4 KFF poll showed 67% parental support, highest among urban millennials at 74%, but dipping to 56% in rural pockets with hesitancy.
Implementation challenges, a soft undercurrent in the policy’s promise, invite thoughtful navigation. Prenatal testing catches 95% of maternal Hep B cases, per ACOG, but 5% gaps remain in uninsured groups, where birth doses avert 90% transmissions. The ACIP’s deferral, with two-month catch-up, sustains 92% herd immunity, per Lancet modeling, but requires outreach—clinics stocking vials, doctors charting statuses. Kennedy pledged $50 million for education, partnering with March of Dimes for multilingual materials. “This is informed families, not forced choices,” he said, his voice a bridge to skeptics. For Carter, home with her son that afternoon, the talk continued: A call to Patel confirming low-risk, a sigh as the two-month slot approached. “It’s scary letting go of routine, but trusting the science feels right,” she said, rocking him under a mobile of stars.
As December’s holidays dawn, with families gathering around tables of stories and shots, the memo stands as recalibration—a nod to evidence that honors birth’s miracle without overwhelming it. For Rahman over tea, Lee in her clinic, and Carter in her nursery, it’s partnership in protection, where vaccines meet vulnerability in care and choice. In America’s tapestry of tiny miracles, this change isn’t rupture; it’s refinement—a gentle adjustment letting families breathe easier, one informed heartbeat at a time.



